Heart failure (HF) is a global public health problem, affecting an estimated 26 million people worldwide and resulting in more than 1 million hospitalizations annually in the US and Europe.1 This HF pandemic is also evident in Asia and other parts of the world.2–4 Although the outcomes for HF patients have improved with the discovery of multiple evidence-based drug and device therapies, hospitalized HF patients continue to experience unacceptably high mortality and readmission rates that have not changed in the past two decades. In parallel with increasing life expectancies worldwide, the proportion of patients with HF is increasing, and an increased percentage of patients are being hospitalized for HF.
Race and Ethnicity in Heart Failure
Race and ethnicity are interrelated concepts that have a long history in the fields of human biology and public health.5 The terms “race” and “ethnicity” are often used interchangeably, and there are no widely-accepted definitions. Race is typically used to refer to groups that share biological similarities; whereas ethnicity refers to shared identity-based ancestry, language and cultural similarities. In many cases, racial and ethnic groups may overlap considerably. Race and ethnicity are useful concepts when attempting to understand differential health risks and health disparities.6 With cardiovascular disease (CVD) accounting for most deaths globally, eliminating racial disparities in cardiac care has become a new challenge in cardiology.7 Furthermore, understanding racial influence in cardiovascular care is important in designing effective measures to eliminate disparities. Traditional risk factors, such as hypertension and ischemic heart disease (IHD), are common in HF patients but vary substantially among the world’s regions.8 It is important to consider these racial differences in the evaluation and management of patients with HF.9 In the US, there are striking differences in the risk factors, incidence, response to treatment and outcomes of HF within each ethnic group. Conventional risk factors, such as hypertension, diabetes mellitus (DM) and IHD, will still predict those at high risk. It is often thought that White Americans tend to develop congestive HF from IHD. For African Americans, hypertension and DM tend to be the primary cause.10 HF affects different racial groups differently, and there are discrepancies in its outcomes as well. Interestingly, the differences in risk factor profiles do not explain the differences in mortality between racial groups. Furthermore, significant racial differences are found in neurohormonal stimulation and pharmacological response in HF. Although most HF treatments are similar, research has demonstrated racial differences in response to therapy. For example, one study suggests that angiotensin-converting enzyme inhibitors are particularly effective in Whites and that hydralazine plus isosorbide dinitrate can be equally effective in Blacks.11
Search Strategy
We conducted a systematic search of published literature in the following online databases: PubMed, Google Scholar, Ovid MEDLINE, Scopus, and Web of Science. Search terms included “race”, “ethnic”, “heart failure”, and “diabetes mellitus.” A large number of trials that have investigated racial differences in HF have been based on studies in the US on African Americans, Hispanic, Chinese American and White participants. The Multiethnic Study of Atherosclerosis (MESA), which started in 2001, was the first large-scale study exploring the role of racial or ethnic differences in heart diseases. Using data from MESA, this review discusses current understanding of the influence of race in the association between DM and HF, the possible mechanisms for these observed differences, and how these may impact on patient management.
Diabetes Mellitus and Heart Failure
The mechanism of HF in patients with DM can be explained by a higher prevalence of risk factors – such as IHD, hypertension, and obesity – and a direct metabolic effect – such as insulin resistance, and increased levels of circulating fatty acids. Both HF and DM are believed to share pathophysiologic processes, including neurohormonal activation, endothelial dysfunction, and increased oxidative stress.12–15
Diabetes Mellitus Predisposes Patients to Heart Failure
DM is an independent risk factor for the development of HF. The Framingham Study revealed a 2.4-fold increase in symptomatic HF in men and a 5.0-fold increase in women with DM, independent of coexisting hypertension or IHD.15 Traditional risk factors for HF – including hypertension, hyperlipidemia, premature atherosclerosis, and left ventricular hypertrophy – occur with increased frequency in the diabetic population and may directly contribute to the development of HF.13,16 DM accelerates the development of atherosclerosis and increases the risk of myocardial infarction and ischemic HF. DM may act synergistically with other risk factors such as hypertension to increase the risk of HF.12 Diabetic cardiomyopathy is a cardiac entity defined as ventricular dysfunction in the absence of coronary artery disease (CAD) and hypertension.14 A US health maintenance study demonstrated that every 1 % increase in baseline glycosylated hemoglobin level correlated with a 15 % increased risk of developing HF.17 DM substantially increases the risk of death, ischemic events and HF,18 particularly in females.19 In the UK Prospective Diabetes Study, poor glycemic control was associated with an increased risk of HF in patients with DM.20
Heart Failure Predisposes Patients to Diabetes Mellitus
In a community-based study, among patients with HF the prevalence of DM increased markedly over time.21 HF itself has been shown to be associated with the development of insulin resistance and new-onset DM. Poorer functional class of HF is associated with the development of DM. Among patients with CAD, advanced heart failure (New York Heart Association class III) is associated with a significantly increased risk (1.7-fold) of developing DM during 6- to 9-year follow-up.22 The higher incidence of hyperglycemia in HF patients with poorer functional class could theoretically be due to either insulin resistance or a greater reduction in the capacity of pancreatic beta-cells to secrete insulin.
Patients with severe HF are more likely to be sedentary. Lack of physical activity in patients with severe HF leads to decreased muscle mass. Muscle is the major site of glucose utilization, and thus a loss of muscle mass increases insulin resistance.
Interactive Effect of Race/Ethnicity and Diabetes in Relation to Heart Failure
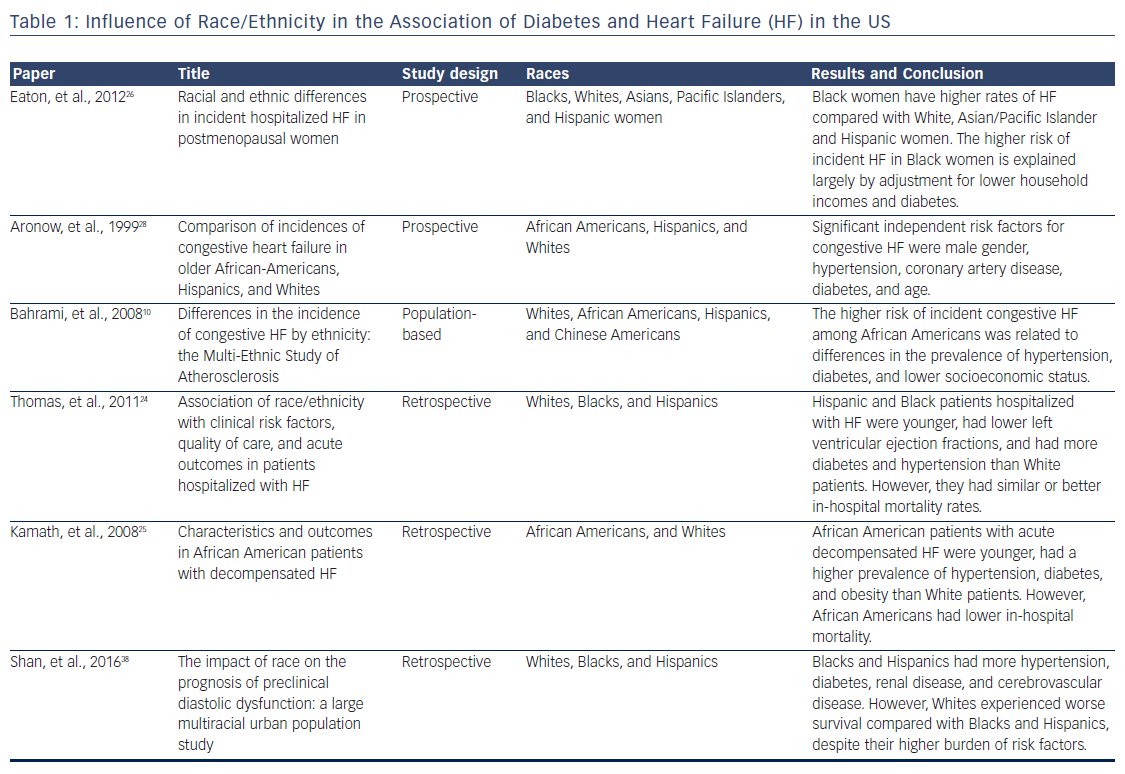
Trials that have examined racial differences in risk factors, the incidence and outcomes of HF in US are shown in Table 1. The main sources of evidence come from observational, retrospective and non-randomized trials.
Risk Factors for Heart Failure
Previous studies have shown a higher prevalence of HF among African Americans, but the reasons for this finding have not been fully understood. A higher burden of risk factors, such as hypertension, DM, a genetic predisposition to cardiomyopathy, and exposure to toxins (including drugs and alcohol), have all been postulated to play a role.23 Subsequently, most work related to racial differences in HF has suggested that differences may be attributable to the relative importance of different risk factors or the issue of access to care.24 Relative to White patients, Hispanic and African American patients were significantly younger, had lower left ventricular ejection fractions, and had more DM, hypertension and obesity.1,24,25
Incidence of Heart Failure
According to a prospective, large, population-based study in the US, African American patients have a significantly higher risk for incident HF compared to White, Hispanic and Chinese American patients.10 In another study of younger patients (<50 years), incident HF was more common among Blacks than Whites.23 A hospital-based study of post-menopausal women involving a multiracial cohort found that Black women had a higher age-adjusted incidence of HF compared to White, Hispanic and Asian/Pacific Islander women.26 This excess risk was explained largely by adjustment for lower household incomes and DM for Black women.26 African Americans and Mexican Americans have approximately double the prevalence of DM compared to White Americans.27 Higher rates of hypertension and DM associated with poverty and other environmental factors, such as high calorie intake among African Americans, largely explain racial differences in the risk of developing HF.10 However, in a multiracial prospective study of 2,893 older people (mean age 81 years) in the US, no significant difference was found in the incident of congestive HF among African Americans, Hispanics, and Whites. The Cox regression model showed that the significant independent risk factors for HF were male gender, hypertension, CAD, DM and age.28
HF with preserved ejection fraction (HFpEF) is an increasingly prevalent condition associated with morbidity and mortality. Clinical manifestations of HFpEF are similar to those observed in HF with reduced ejection fraction. Researchers found that the incidence rates of HFpEF were similar across all races (Whites, Blacks, Hispanics and Chinese). Risk factors such as age, hypertension, DM and BMI were significant predictors of incident HFpEF.29 Outside the US, a UK study involving 1 million patients that focused on racial differences in the lifetime presentation of CVD found no differences in initial presentation with HF between White, South Asian and Black patients.30 Unlike the US studies, Black patients in this study had rates of hypertension comparable to White patients. A population-based study in the US examining diabetic cardiomyopathy using cardiac magnetic resonance imaging of individuals from four ethnic groups (White, African American, Hispanic and Chinese) found that end diastolic volume and stroke volume were reduced, and left ventricular mass was increased in Blacks with DM. This study concluded that ethnicity-specific differences in left ventricular mass, end diastolic volume, and stroke volume were associated with abnormal glucose metabolism and were independent of subclinical CVD.31 Another interesting study from the MESA group showed that NT-proB natriuretic peptide concentrations differed significantly by race. Natriuretic peptides are cardiac-derived hormones with favorable cardiometabolic actions. Low natriuretic peptide levels are associated with increased risks of hypertension and DM. In multivariable models, NT-proB natriuretic peptide levels were lower in Black and Chinese people compared with Whites. Hispanics had intermediate hormone concentrations.32
Progression of Heart Failure
Racial differences play an important role in the progression from asymptomatic left ventricular dysfunction to congestive HF. In the Studies of Left Ventricular Dysfunction (SOLVD), African Americans with mild to moderate left ventricular systolic dysfunction were at higher risk for progression to HF than Whites.33 The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) recently identified this group as a population at high risk for the development of clinical HF.34 Hispanics/Latinos are particularly vulnerable to cardiac dysfunction because they have an increased prevalence of risk factors for HF, with higher rates of DM, obesity and hypertension.35–37 Half of the participants in HCHS/SOL were obese or hypertensive, and two-thirds had DM or were pre-diabetic. Cardiac dysfunction was present in almost half of the cohort and was due predominantly to diastolic dysfunction. Furthermore, of all cardiac dysfunction, upwards of 95 % was unrecognized or subclinical.
A study was performed to assess the impact of race in patients with preclinical diastolic dysfunction. Despite Blacks and Hispanics having more hypertension, DM, renal disease, and cerebrovascular disease than Whites, time to HF was similar among the three racial groups.38
Outcomes of Heart Failure
African Americans are more likely to be readmitted to hospital, to spend longer in hospital and to have higher hospital costs (reflecting more complex and difficult-to-treat conditions), as well as being less likely to be treated by cardiologists, suggesting worse access to and quality of care than other racial groups.39 These differences are likely related to socioeconomic and behavioral characteristics, including disparities in access to and quality of health care, as documented by congestive HF morbidity and mortality studies.40 The difference in the risk factor profile was unable to explain the differences in mortality between racial groups. Despite the higher burden of risk factors (DM, hypertension and obesity) and lower ejection fraction among African American and Hispanic HF patients, Whites experienced similar or worse survival after adjustment for known predictors.24,25,38,41,42 Future studies are required to improve our understanding of the impact of mechanisms of race on HF outcomes.
There are numerous published data on HF and ethnicity outside the US focusing on different racial groups. The simplified review below provides a glimpse of the epidemiological differences in HF in different geographic regions of the world.
A retrospective cohort study that was conducted on 4.7 million people in Scotland to determine the incidence of first HF hospitalization or death by racial group found that South Asians (Pakistani men and women) had a higher risk ratio than White British and Chinese.43 In the Middle East, a study involving seven Arabian Gulf states (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, the United Arab Emirates, and Yemen) reported that acute HF patients from this region were a decade younger than their Western counterparts, with a high prevalence of IHD and DM, and a higher risk of acute HF with reduced ejection fraction.44 In Africa, acute HF has a predominantly non-ischemic cause, most commonly hypertension. The condition occurs in middle-aged adults, affects men and women equally, and is associated with high mortality. The outcomes are similar to those observed in non-African acute HF registries, suggesting that acute HF has a dire prognosis globally, regardless of the cause.45
In Asia, recent increases in cardiovascular risk factors have contributed to a particularly high burden of HF, with outcomes that are poorer than those in the rest of the world. HF hospitalizations are on the rise and, compared with Western counterparts, HF occurs at a younger age. It is characterized by more severe clinical features and worse outcomes in south-east Asian patients.3 The at-risk population is increasing at a faster rate in Asia than in other parts of the world, and reflects increases in the prevalence of CAD, hypertension, DM, obesity, and tobacco use. Prospective multi-national data highlight the significant heterogeneity among Asian patients with stable HF, and the important influence of both race and regional income level on patient characteristics. The prevalence of DM is highest in south-eastern Asians and lowest in north-eastern Asians, with notable geographic and racial variations.2
South-east Asian countries, such as Malaysia and Singapore, consist of multiracial Asians (Malay, Chinese, Indian and other ethnic minorities); an ideal population to use when exploring racial variations in CVDs. Compared to other regions of Asia, south-east Asia has the greatest burden of risk factors (hypertension and DM).2 The adjusted odds ratio of DM was 4.9 higher in Indians compared to Malays and Chinese, particularly in high-income regions.2 In Malaysia, a prospective survey of congestive HF in a single center showed variations in associated etiological factors between racial groups. CAD was the main etiology of HF, followed by hypertension. DM was the risk factor affecting the majority of Indians as compared to Malays and Chinese.46 A higher rate of DM in Indians compared to other races has been confirmed by studies and multi-center registries worldwide.47–50 A prospective observational study consisting of the multiracial population in Singapore showed that Indian and Malay patients had worse HF outcomes than Chinese patients. These differences were attributed to a greater prevalence of DM among Indians. However, the cause of the poorer prognosis in Malays is unclear in this study.51 There are more data on racial differences in HF in different parts of the globe, however these data are beyond the scope of current review.
In the authors’ opinion, patients with DM have higher rates of HF due to its adverse effects on endothelial dysfunction, altered metabolism and increased oxidative stress, clustering with other predisposing risk factors (DM and hypertension) that accelerate the development of atherosclerosis and increase the risk of IHD.12–14,16 If the predisposing risk factors are more prevalent in any racial group, they will increase the incidence of HF.2,10 We also think that the outcomes of HF may be influenced by the control of DM, regardless of racial differences. If diabetes control is poor due to low educational status, access-to-care or socioeconomic issues, we believe this will have direct impact on mortality rate regardless of racial background. The current review reinforces the need for optimal control of DM to effectively reduce the increasing social burden of HF.
Conclusions
The interaction between race and DM carry important public health implications for the management and prevention of HF. African American patients in the US have a significantly higher incidence of HF, lower ejection fraction, and are younger at presentation compared to White, Hispanic and Chinese American patients. These findings are largely explained by the higher burden of risk factors such as DM, hypertension, obesity, and lower household incomes among African Americans. The authors believe that these findings are applicable to other racial groups. The prevalence of predisposing risk factors probably has a stronger influence on the incidence of HF than the racial factor alone.







